Making Healthcare Equitable in 2023

In 2023, providers and employers understand that it’s critically important to recognize and tackle persistent health disparities to improve access and outcomes for everyone.
But new requirements from the federal government mean addressing health equity is becoming even more urgent and necessary.
Under the new ACO REACH payment model, participants will be required to meet several provisions on promoting health equity, including the creation of a health equity plan and the collection of health equity data to determine social risk factors.
It’s estimated that 80% to 90% of health outcomes are dictated by social determinants of health, including employment status, education, housing, transportation, dietary habits and more. Pain impacts everyone, but not everyone gets the care that they need to overcome it.
Today, disproportionate health outcomes paint a tragic picture of discrimination in healthcare. Why? Persistent disparities stand in the way of quality treatment and achieving ideal health.
As a solution for overcoming musculoskeletal (MSK) pain, we at Sword Health have seen firsthand how underserved and minority populations face entrenched barriers to care, and how they experience worse health outcomes because of it. We developed a digital health program with the goal of bringing lasting pain relief to as many people as possible—regardless of their background, where they live, or how much they earn.
Here are four key ways to actively dismantle disparities in healthcare.
#1: Broadening access to care with innovative technology
Today, digital healthcare alternatives have a unique power. The convenience of at-home care encourages a trend of unprecedented engagement: one where more people heal. Indeed, Sword was first in the industry to prove that a digital physical therapy program could drive the same and better outcomes than traditional, in-clinic treatment. Our Digital Therapist allows members to perform their prescribed exercises at a time and place of their choosing — all under the supervision of licensed doctors of physical therapy. There’s no need to book an appointment, drive to the clinic, or take time off work, which all contribute to 70% of PT patients never finishing their prescribed treatments.
We know that Black, Hispanic and minority patients do not access telehealth as much as their Caucasian counterparts. They’re more likely to visit the emergency room or make an in-clinic visit instead of using a telehealth service. Across the board, they experience worse health outcomes than white patients, including after rehabilitation. Digital care options have the potential to change all that. Increased convenience, accessibility, and adherence leads to better outcomes for these historically underserved groups.
#2: Offering low-cost options to expensive interventions
When it comes to income-based disparities in health, the United States has some of the worst outcomes. Americans who are poor are nearly five times as likely to be in bad or only fair health when compared with people who are affluent. They’re also three times more likely to limit their physical activity due to chronic illness.
To combat some of these income-based barriers, digital healthcare solutions are innovating ways to become available at no cost to most members. By partnering with employers, labor unions, and health plans, digital healthcare companies offer support as a workplace benefit with zero out-of-pocket costs. This model ensures that the people who are most in need of high-quality, affordable physical care can get it without financial burden.
For solutions like Sword, we boldly aspire to steer members away from expensive, invasive interventions such as back and knee surgery. Instead, our digital program relies on the proven benefits of physical therapy: the mainstay, non-invasive treatment for MSK pain that also happens to be more effective than surgery in most cases. This is crucial because studies show that Black and Hispanic populations are more at risk for receiving low-quality tests and treatments, such as inappropriate imaging for low-back pain.
By making virtual physical therapy available to all, Sword prevents unnecessary surgeries and gives everyone equal access to best-in-class treatment options—at no cost to members.
#3: Eliminating the hurdle of transportation
Transportation has been shown to be a major barrier to healthcare access, especially for low-income earners and people living in rural areas. The burden and cost of getting to a healthcare provider or facility can lead to missed appointments, delayed care, unmet health needs, exacerbation of chronic conditions, and generally poorer health outcomes. In fact, each year, nearly 4 million people in the U.S. do not obtain medical treatment due to transportation issues.
Indeed, even internet access can be a problem for the 1 in 5 patients who reside in rural areas. The convenience of digital care means members get help without disrupting their lives. For many working-class individuals, this is the difference between getting the care they need and the alternative—continuing to live in pain.
At Sword, our program is designed to provide 24/7 access to therapy, eliminating the barriers such as taking time off from work, or traveling to get treatment. In fact, up to 48% of our member sessions occur between 6 pm and 8 am, and 22% take place on weekends. When most clinics are closed, Sword is available. Sword also provides hotspots at no cost to members who don’t have access to reliable, high-speed Internet service, a common problem in rural areas.
#4: Delivering personalized care that addresses each member’s needs
Systemic racism exists in healthcare. It sustains health inequities within communities of color that put these populations at greater risk of illness and death across a wide range of conditions, including MSK disorders. Racism denies an individual’s humanity, value and uniqueness. To mitigate disproportions in care, it’s important that care is tailored specifically to the individual — taking into account their experience, race, ethnicity, language, and ability to perform. And that care must be ongoing.
Backed by a diverse team of physical therapists, Sword is built on delivering personalized care tailored for each member’s specific goals, challenges, and environment. Each member is matched with a dedicated doctor of physical therapy who guides them through 100% of their treatment, so they never feel alone on their healing journey. Approximately a quarter of our PTs come from underrepresented minority groups and 11% are bilingual or multilingual. Every PT receives sensitivity training from organizations such as PT Proud to build equitable values. We want our members to see themselves in our program so they feel comfortable getting the treatment that they need.
At Sword, our goal is to eliminate as many obstacles to a pain-free life as possible for our members. This cannot be done without recognizing that many people face unjustified barriers to getting good care, and without the strongest commitment to overcoming entrenched health disparities—in action, not just words. We cannot overcome pain without also striving to overcome systemic inequities in every way.
How we’re improving health equity today
Black and Hispanic patients come to healthcare providers with more severe pain and disability than the average patient. This is true throughout the healthcare sector. Unfortunately, in traditional healthcare, these are the patients who also experience the worst outcomes. They generally don't make the same gains as white and Asian patients.
However, with a digital solution like Sword, we’ve discovered proven ways to overcome the barriers of time, transportation and cost, and dramatically improve the outcomes that historically present in Black and Hispanic patients. Indeed, with Sword, these groups were more likely to achieve a 30% improvement in their pain scores.
In the first study of its kind on the impact of racial differences on outcomes in digital MSK care, we were able to demonstrate that by overcoming social determinants of health barriers, we can truly equalize health outcomes for Black and Hispanic groups.
We found that these patients had higher MSK burden at baseline (as shown in previously published data), but incredibly higher likelihood of pain improvement. The outcomes were so outstanding, by the time Black and Hispanic patients finished Sword, pain and disability levels were similar across all racial and ethnic backgrounds.
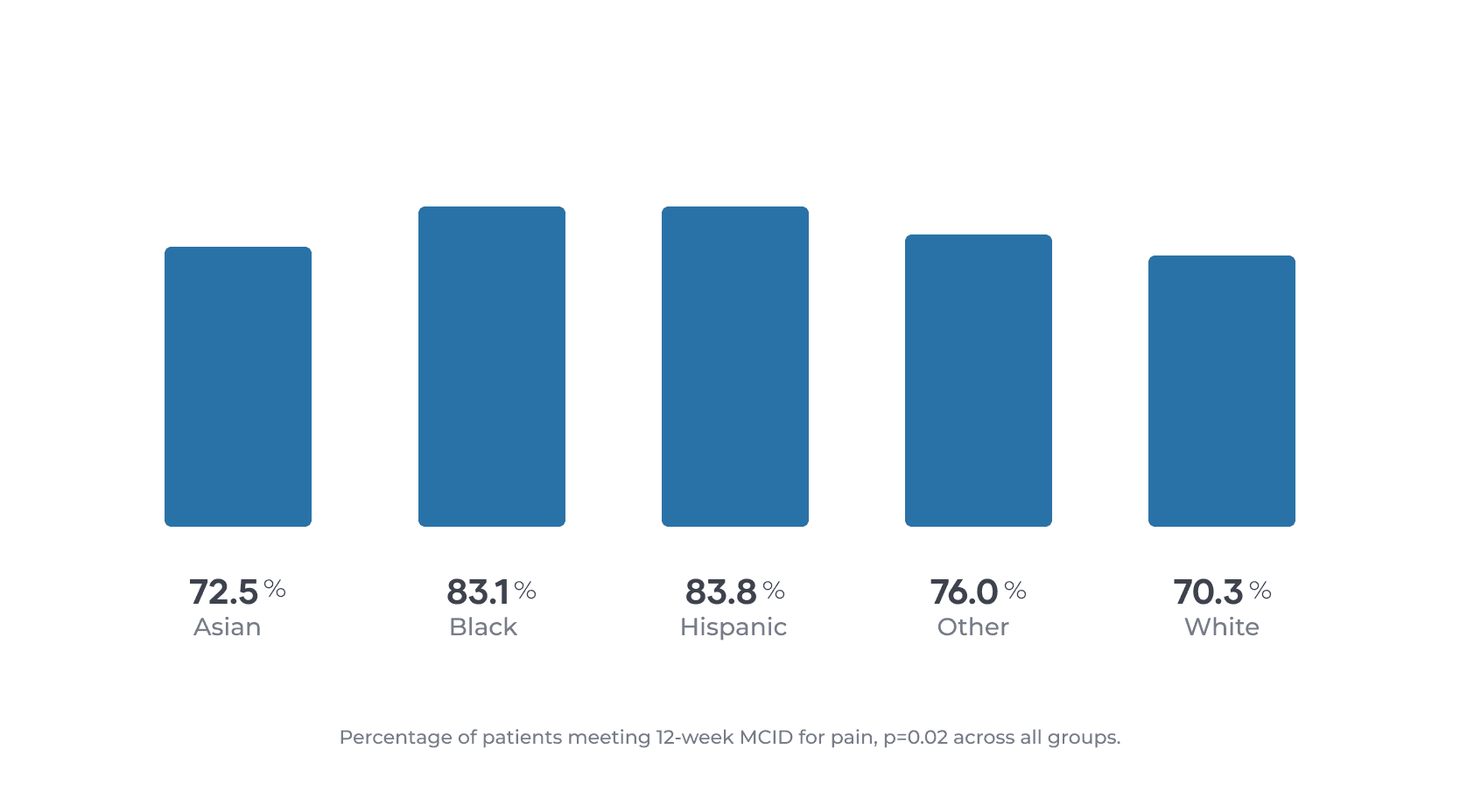
The results buck against published literature showing that minority groups generally have worse outcomes when going through rehabilitation programs. This provides further evidence that Sword’s digital program can drive substantial health improvements in communities that have historically experienced poor outcomes.
The cohort of 6,949 patients was diverse, and had a racial and ethnical mix similar to the proportions of the general U.S. population. It’s the first peer-reviewed study to specifically assess the impact of race on engagement and outcomes with patients using a virtual MSK program.
It also demonstrates Sword’s tremendous value in improving access to MSK care and promoting health equity among historically underserved populations.

